
Background:
The following is an overview of an actual case of a woman in her mid-forties with a college degree working in the technical field. Her name and all identifying information have been changed to protect her anonymity. This case highlights the value of the MOX0 d-CPT in providing important neuropsychological data that cannot be collected by any other means of assessment.
Screening
Eight months prior to this neuropsychological evaluation, Mary was involved in an automobile accident. While passing through an intersection her vehicle was hit broad side by a vehicle that had failed to stop for a red light. At the scene, Mary was unconscious for a brief period of time as reported by onlookers. When EMT arrived she was awake but repetitively questioning. Mary was the driver and the airbags in her vehicle had deployed. In the hospital emergency room she was diagnosed with a concussion and multiple strains and sprains. She was kept overnight for observation. Subsequent brain imaging did not reveal signs of bleed nor other severe brain trauma.
In the first two weeks following this accident, Mary developed a full constellation of post- concussive symptoms. She appeared extremely fatigued, suffered from a constant headache, reported that her body ached, slept an extensive amount of time and seemed notably unfocused to her spouse when awake.
Two weeks post-injury, Mary attempted to return to work but struggled with fatigue, problems with concentration and memory for routine activities. She was released from world for another period of a few weeks, eventually able to return but at the time of the evaluation reported she was struggling with efficiency, organization, concentration and memory at work. Her persistent, constant headache eventually remitted after approximately two to three weeks. However, she now began experiencing daily headaches that tended to start mid -day and progress in severity throughout the day. These were subsequently diagnosed as post traumatic migraine. Mary was prescribed medication with some reported benefit.
Approximately two months post-accident, a cervical spine MRI yielded impressions of multiple disk problems that was attributed to injuries from the accident. Mary at that time reported suffering from daily, nearly continuous chronic pain in her back and disruptive sleep due to pain.
During the history taking of the assessment, Mary reported continued problems with headache, cervical pain, challenges with sleeping, problems with concentration and short term memory, excessive emotionality, irritability and an adverse sensory change, including being bothered by noises, odors and bright lights. Mary’s persistent symptoms now met the criteria for a Persistent Post Concussive Disorder. She reported problems with work, community activities and meeting daily responsibilities. Her self-reports reflected difficulty with behaviors related to attention, executive function and mood regulation.
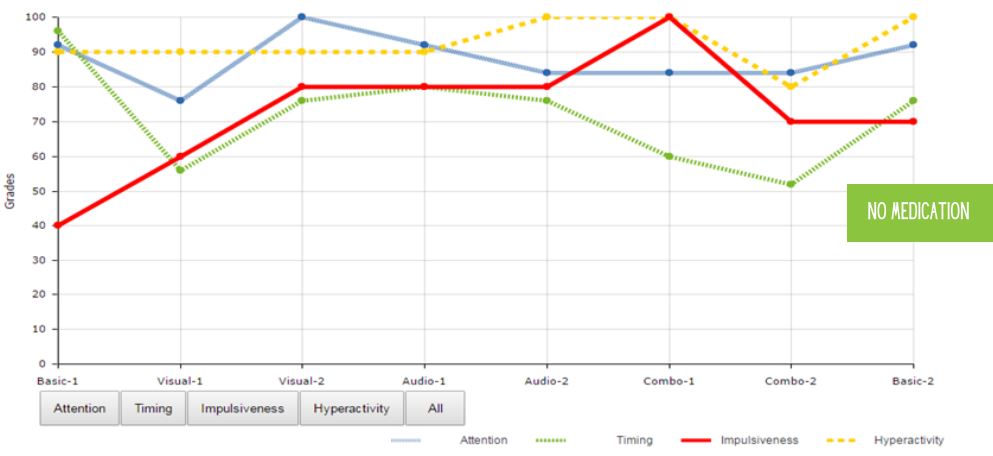
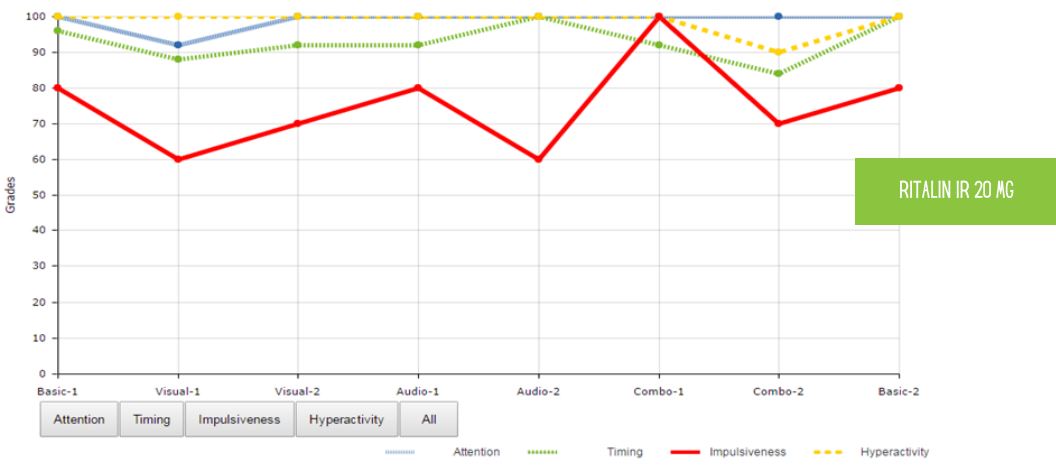
During the administration of a neuropsychological test battery, Mary worked diligently. There was no indication that she lacked effort or motivation. Her above average measured intellect and reading abilities provided strong foundation that she had likely functioned in this range life time. These scores were consistent with her excellent college grades and her work history. In contrast, testing demonstrated problems with short term working memory and the speed with which Mary could respond to and process information, particularly on a broad memory battery. Mary’s MOXO scores appear below:
Summary
The MOXO scores very clearly demonstrate a decline in Mary’s timeliness or ability to process through the task at a level consistent with her intellect and capacity to pat attention. The sensativity of the finding on a computerized measure adds further data to the rest of the neuropsychological test battery. Mary also reported full set of symptoms related to Post Traumatic stress disorder. She was anxious when driving, preferred not to drive and was experiencing periodic night mares concerning the accident. Her personality profile reflected someone absent a history of mental health personality or personality problem but currently experiencing an acute onset of anxiety symptom related to the accident.
Mary’s presentation appeared consistent for an individual suffering from persistent post concussive disorder. In Mary’s case, specific problems with speed of processing leading to difficulty with working memory and capacity to learn new information was and continued to be impaired post accident. In this case,
the MOXO provided supportive evidence of Mary’s traumatic brain injury.





